About Your Tooth
Your tooth consists of two main parts:
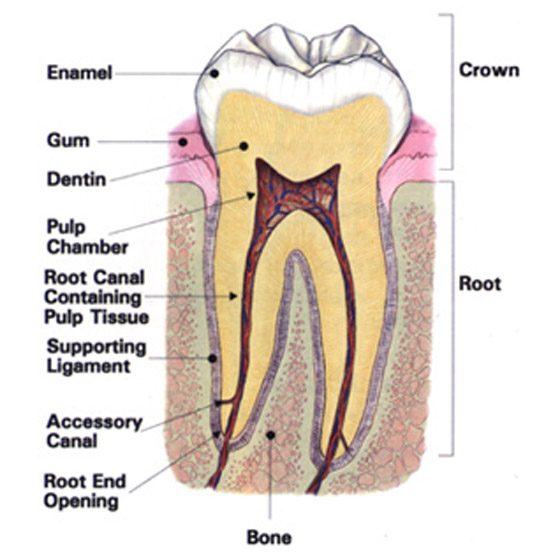
- The Crown, which is that part of the tooth above the gum and visible in your mouth;
- The Root(s), which is that part of the tooth that lies beneath the gum and is surrounded by bone. Inside each root is a channel that runs the length of the tooth called the root canal. This contains the pulp (nerves, blood vessels, and soft tissue) and is often referred to as the “nerve” of the tooth.
What is Endodontics?
In order to preserve a tooth that is ‘dying’, it is necessary to remove the infected and inflamed pulp tissue from inside the roots to prevent further spread into the surrounding tissues. The roots are then filled and sealed. This procedure is known as endodontic or root canal therapy. Endodontic therapy is concerned with removing only the pulp from the root canal, so the root and tooth will remain intact and continue to function normally in jaw bone after the treatment.
Afterwards, you return to your own general dentist who will place a permanent filling and crown on the tooth to protect it’s long-term function.
Who performs Endodontics?
 Your own general dentist has received basic training in endodontics during their degree course at dental school. BUT they may refer you to a Specialist Endodontist due to the complexity of an infected tooth or simply to ensure maximum predictability of health of the tooth if expensive, cosmetic, or complex restorations are to be made.
Your own general dentist has received basic training in endodontics during their degree course at dental school. BUT they may refer you to a Specialist Endodontist due to the complexity of an infected tooth or simply to ensure maximum predictability of health of the tooth if expensive, cosmetic, or complex restorations are to be made.
Endodontists have completed formal University-based postgraduate training. Dr Bhanderi is registered as a Specialist in Endodontics with the General Dental Council.
Why?
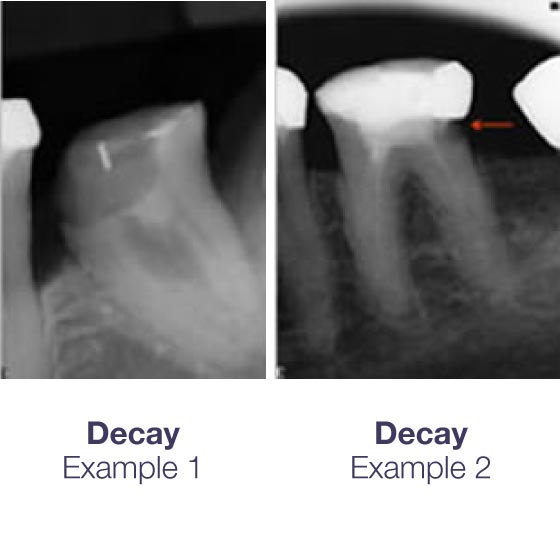 This pulp may become irreversibly damaged because of infection associated with decay, very deep fillings, repeated dental procedures, a crack in the tooth, trauma, or advanced periodontal (gum) disease. Once it has been confirmed that the pulp is irreversibly damaged then the pulp must be removed and the root canals thoroughly cleansed, disinfected, and filled.
This pulp may become irreversibly damaged because of infection associated with decay, very deep fillings, repeated dental procedures, a crack in the tooth, trauma, or advanced periodontal (gum) disease. Once it has been confirmed that the pulp is irreversibly damaged then the pulp must be removed and the root canals thoroughly cleansed, disinfected, and filled.
Decay – When decay in a tooth becomes so extensive that it penetrates into the pulp of the tooth, then the bacteria that are associated with the decay infect the pulp. Eventually, the pulp and all its contents will become inflamed (sometimes causing pain) and will die. The infection will then spread throughout all the root canals and may seep out through the end of each root into the surrounding jaw bone.
Pain and Swelling – If the infection is left untreated for a considerable time then it will percolate through the end of the roots and cause an infection in the jaw bone. Sometimes this is very aggressive, called an abscess. Other times it can remain quiescent, slowly destroying the jaw bone at the end of the infected roots. It may then spread up the side of the tooth’s roots and infect the supporting bone and gums, with or without any symptoms.
How?
The whole procedure is performed under complete local anaesthesia, so you will feel no pain and will always be awake. If at any time you feel discomfort, I will stop immediately and identify the cause and try and alleviate it. We then will ‘isolate’ the tooth by wrapping it up with a clip and rubber sheet (a ‘rubber dam’).
This prevents any water, debris, filling materials, and some of the unpleasant tasting materials that we use from falling to the back of your mouth and throat. As we treat the tooth, you can swallow normally and move your tongue around under the rubber dam and we won’t need to stick a suction device into your mouth or down your throat! It may feel a little weird initially but you will quite quickly feel comfortable with it and most importantly it doesn’t hurt at all!
Under an operating microscope, we will then just remove any old fillings and decay, and then explore for all the possible root canals. Once all are found, each root canal is then cleaned and disinfected right to the natural end of the tooth before filling.
When?
 Signs and symptoms to look for include prolonged and spontaneous pain, prolonged sensitivity to cold but especially to hot, swelling and tenderness in the overlying gums, and sometimes discoloration of the tooth. But occasionally there may be no other obvious symptoms.
Signs and symptoms to look for include prolonged and spontaneous pain, prolonged sensitivity to cold but especially to hot, swelling and tenderness in the overlying gums, and sometimes discoloration of the tooth. But occasionally there may be no other obvious symptoms.
If the tooth looks too infected at the first visit or there have been problems in identifying or cleaning all the root canals, then the tooth will be filled with an antiseptic dressing and you will need to return for another appointment for the final root-filling.
Usually, the whole appointment will last for between 1-1½ hours. I will keep you informed throughout the procedure.
Occasionally, we may want to review the tooth after the root filling has been done on a 6-monthly basis in order to monitor your healing response. These appointments are very important as they allow us to intervene swiftly if the situation appears to be deteriorating. These review appointments are very short and simply involve looking at the tooth and taking an x-ray to see how well the bone and gums are healing. There is usually no further charge to you for these short review appointments.
 Usually we will ask your own dentist to keep an ‘eye on things’.
Usually we will ask your own dentist to keep an ‘eye on things’.
Immediate Post-treatment Care Guides
For the first few days after treatment the tooth may feel a little ‘achy’, especially if there was pain or infection before the procedure.
This discomfort is sometimes caused by the fact that we have instrumented and disturbed the infected area just outside the end of the roots and the pressure of applying the root-filling. This can be relieved with over-the-counter or prescription medications.
Evidence shows that taking an anti-inflammatory just before and after the treatment (e.g. 400 mg Ibuprofen, “Nurofen Plus”), or if you have a medical condition that precludes you taking his type of painkiller (e.g. asthma, gastric ulcer), then 1000mg Paracetomol will help in minimising the discomfort.
If you have had endodontic treatment, download Endo61 post-treatment information here:

Others Causes of ‘Toothache’